Optimal therapy for improved patient care and better outcomes

Optimal therapy for improved patient care and better outcomes
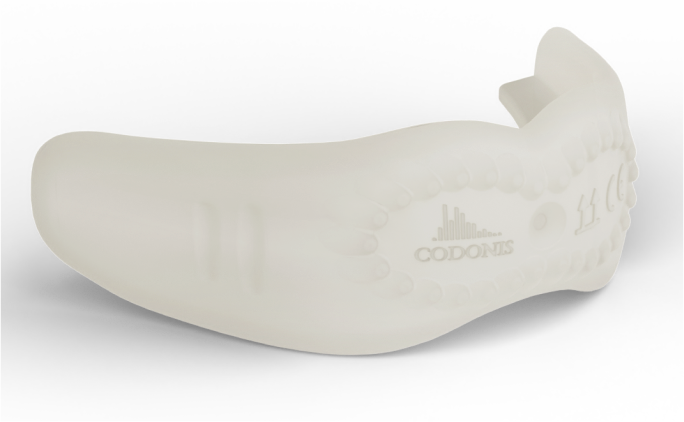
Unique Surface Design
The CODONIS LWZ has a unique surface- the front surface has a special design to stimulating the adjacent soft tissue respectively muscules by specific nubs
Versatile Design
The CODONIS LWZ is designed in a nique way to fit children with primary dentition up to seniors
Positioning
To keep the CODONIS LWZ in place, the device is equiped with bite rails.
CODONIS-App
Unique platform for personalization of CODONIS LWZ with therapy plan

The CODONIS LWZ has a unique surface- the front surface has a special design to stimulating the adjacent soft tissue respectively muscules by specific nubs
The CODONIS LWZ is designed in a nique way to fit children with primary dentition up to seniors
To keep the CODONIS LWZ in place, the device is equipped with bite rails.
Unique platform for personalization of CODONIS LWZ with therapy plan
Within the adoption phase, the use of the device is steadily increased.
During the intensive phase the therapists encourages the patient to use the CODONIS LWZ for a prolonged therapy time interval.
Within the fade out phase, the therapy durations are steadily reduced
Patient recalls are made to ensure that there are no recurrences, generally after 1, 3 and 6 months since the last use.
Easy – in a few steps the CODONIS LWZ is on its ways


Ahmad, M. and Schiffman, E.L. (2016) ‘Temporomandibular Joint Disorders and Orofacial Pain’, Dental clinics of North America, 60(1), pp. 105–124. Available at: https://doi.org/10.1016/j.cden.2015.08.004
D’Onofrio, L. (2019) ‘Oral dysfunction as a cause of malocclusion’, Orthodontics & Craniofacial Research, 22 Suppl 1(Suppl 1), pp. 43–48. Available at: https://doi.org/10.1111/ocr.12277
Grabowski, R., Kundt, G. and Stahl, F. (2007) ‘Interrelation between occlusal findings and orofacial myofunctional status in primary and mixed dentition: Part III: Interrelation between malocclusions and orofacial dysfunctions’, Journal of Orofacial Orthopedics = Fortschritte Der Kieferorthopadie: Organ/Official Journal Deutsche Gesellschaft Fur Kieferorthopadie, 68(6), pp. 462–476. Available at: https://doi.org/10.1007/s00056-007-0717-y
Huber, Bettina (2017) Wirkungsweise des Lippen-Wangen-Zungen-Trainers (LWZ-Trainers) auf das infantile Schluckmuster (Pilotstudie). Master Thesis. Klinik für Mund -, Kiefer- und Gesichtschirurgie Universitätsspital Basel.
Koka, V. et al. (2021) ‘Orofacial Myofunctional Therapy in Obstructive Sleep Apnea Syndrome: A Pathophysiological Perspective’, Medicina, 57(4), p. 323. Available at: https://doi.org/10.3390/medicina57040323
Pizolato, R.A., Freitas-Fernandes, F.S. de and Gavião, M.B.D. (2013) ‘Anxiety/depression and orofacial myofacial disorders as factors associated with TMD in children’, Brazilian Oral Research, 27(2), pp. 156–162. Available at: https://doi.org/10.1590/s1806-83242013000100021
Ray, J. (2006) ‘Orofacial myofunctional deficits in elderly individuals’, The International Journal of Orofacial Myology: Official Publication of the International Association of Orofacial Myology, 32, pp. 22–31.
Seemann, J., Kundt, G. and Stahl de Castrillon, F. (2011) ‘Relationship between occlusal findings and orofacial myofunctional status in primary and mixed dentition: part IV: interrelation between space conditions and orofacial dysfunctions’, Journal of Orofacial Orthopedics = Fortschritte Der Kieferorthopadie: Organ/Official Journal Deutsche Gesellschaft Fur Kieferorthopadie, 72(1), pp. 21–32. Available at: https://doi.org/10.1007/s00056-010-0004-1
Streff, Susanne (2017) Evaluation der Wirkweise des Lippen-Wangen-Zungen-Trainers auf die orofaziale Muskulatureine prospektive Pilotstudie bei Erwachsenen aus logopädischer Sicht. Master Thesis. Klinik für Mund-, Kiefer- und Gesichtschirurgie Universitätsspital Basel.
Sude, A. et al. (2021) ‘Temporomandibular Disorder Related Characteristics and Treatment Outcomes in Oromandibular Dystonia Patients in Two Different Clinical Settings: A Cross-Sectional Study’, Journal of oral rehabilitation, 48(5), pp. 542–550. Available at: https://doi.org/10.1111/joor.13162
We recommend to use the CODONIS LWZ for a standard cycle of about 3 month. After this time the CODONIS LWZ should be replaced
The CODONIS LWZ can be used wherever the patient is. The patient should make sure he cleans the hands prior use of the device for hygienic reasons
Yes, you can.
This depends on the patient and the ability to use the CODONIS LWZ. It may be advisable to accommodate the device with kids or disabled person first and then – as per routine plan- perform the therapy.
CODONIS is a Swiss based company which develops and markets innovative and forward-looking medical products for logopedics, myofunctional therapy and dentistry.
Office:
Tramstrasse 99, 4132 Muttenz, Switzerland
Email:
contact@codonis.ch
VAT: CHE-316.119.424
Ahmad, M. and Schiffman, E.L. (2016) ‘Temporomandibular Joint Disorders and Orofacial Pain’, Dental clinics of North America, 60(1), pp. 105–124. Available at: https://doi.org/10.1016/j.
D’Onofrio, L. (2019) ‘Oral dysfunction as a cause of malocclusion’, Orthodontics & Craniofacial Research, 22 Suppl 1(Suppl 1), pp. 43–48. Available at: https://doi.org/10.1111/ocr.
Grabowski, R., Kundt, G. and Stahl, F. (2007) ‘Interrelation between occlusal findings and orofacial myofunctional status in primary and mixed dentition: Part III: Interrelation between malocclusions and orofacial dysfunctions’, Journal of Orofacial Orthopedics = Fortschritte Der Kieferorthopadie: Organ/Official Journal Deutsche Gesellschaft Fur Kieferorthopadie, 68(6), pp. 462–476. Available at: https://doi.org/10.1007/
Huber, Bettina (2017) Wirkungsweise des Lippen-Wangen-Zungen-Trainers (LWZ-Trainers) auf das infantile Schluckmuster (Pilotstudie). Master Thesis. Klinik für Mund -, Kiefer- und Gesichtschirurgie Universitätsspital Basel
Koka, V. et al. (2021) ‘Orofacial Myofunctional Therapy in Obstructive Sleep Apnea Syndrome: A Pathophysiological Perspective’, Medicina, 57(4), p. 323. Available at: https://doi.org/10.3390/
Pizolato, R.A., Freitas-Fernandes, F.S. de and Gavião, M.B.D. (2013) ‘Anxiety/depression and orofacial myofacial disorders as factors associated with TMD in children’, Brazilian Oral Research, 27(2), pp. 156–162. Available at: https://doi.org/10.1590/s1806-
Ray, J. (2006) ‘Orofacial myofunctional deficits in elderly individuals’, The International Journal of Orofacial Myology: Official Publication of the International Association of Orofacial Myology, 32, pp. 22–31.
Seemann, J., Kundt, G. and Stahl de Castrillon, F. (2011) ‘Relationship between occlusal findings and orofacial myofunctional status in primary and mixed dentition: part IV: interrelation between space conditions and orofacial dysfunctions’, Journal of Orofacial Orthopedics = Fortschritte Der Kieferorthopadie: Organ/Official Journal Deutsche Gesellschaft Fur Kieferorthopadie, 72(1), pp. 21–32. Available at: https://doi.org/10.1007/
Streff, Susanne (2017) Evaluation der Wirkweise des Lippen-Wangen-Zungen-Trainers auf die orofaziale Muskulatureine prospektive Pilotstudie bei Erwachsenen aus logopädischer Sicht. Master Thesis. Klinik für Mund-, Kiefer- und Gesichtschirurgie Universitätsspital Basel.
Sude, A. et al. (2021) ‘Temporomandibular Disorder Related Characteristics and Treatment Outcomes in Oromandibular Dystonia Patients in Two Different Clinical Settings: A Cross-Sectional Study’, Journal of oral rehabilitation, 48(5), pp. 542–550. Available at: https://doi.org/10.1111/joor.